Chronic Care Management
Outcome-driven and Evidence-based Chronic Care Management Solution
The State of Chronic Care
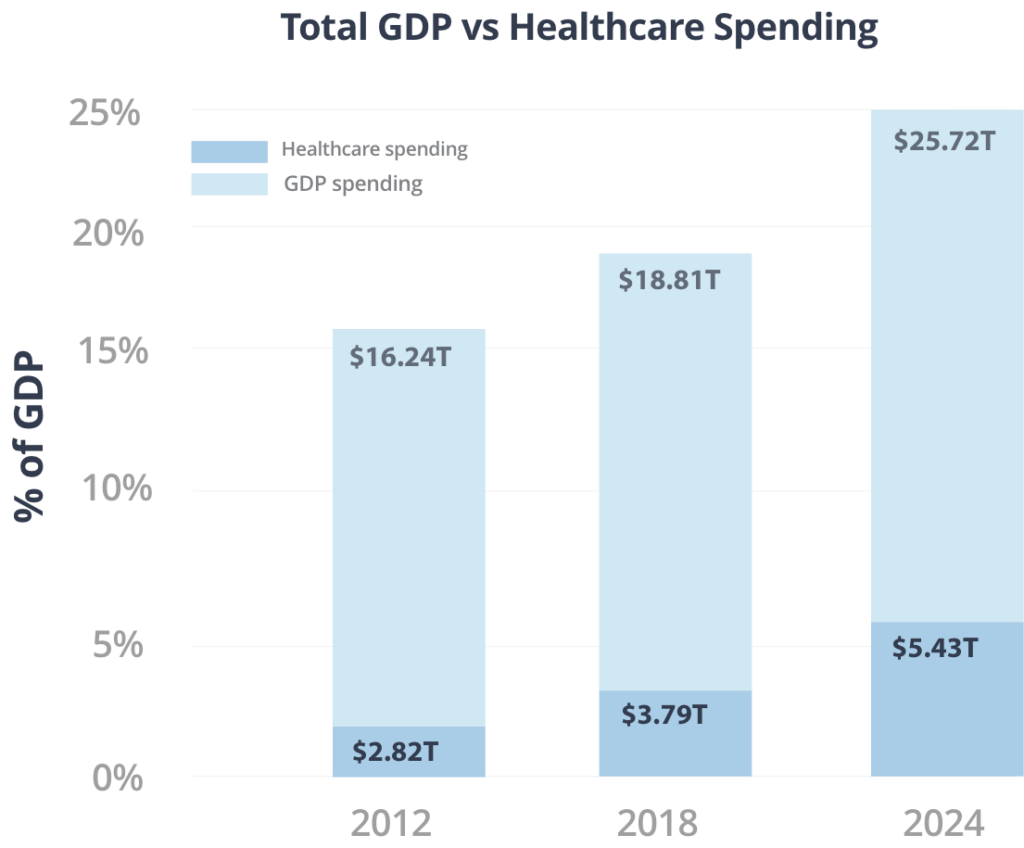
In America’s fragmented healthcare system, millions of people with chronic conditions desperately need coordinated care. Chronic conditions account for nearly 86% of U.S. healthcare spending, and continue to grow.
Challenges of Implementing Chronic Care Management
Limited time and practice resources
Uncertain financial success
Worries over red-tape and changing CMS rules
Requires investment in technology
PharmD Live® improves patient outcomes and drives clinical efficiency and value-based care profitability
Streamlined practice onboarding for fast program start-up
Enrollment process maximizes patient participation
Dedicated clinical pharmacists handle patient encounters
Medication management expertise
Proven telehealth technology with predictive analytics
Find out how PharmD Live can integrate our CCM solution with your practice
PharmD Live CCM solutions enable physicians to deliver the highest quality care for their patients with chronic conditions
- PharmD Live’s Chronic Care Management (CCM) telehealth solution seamlessly integrates with physician practices and healthcare systems to provide care coordination, medication management and consistent patient engagement.
- PharmD Live alleviates physician workload and improves MIPS and APMS quality scores by billing CPT codes 99490, 99487, 99489, 99491 and G2058.
Download the Overview and Guide to Improving Patient Health Outcomes with Interdisciplinary Services
A personalized, evidence-based and convenient approach to chronic care
Your patients will appreciate our structured CCM program that addresses Social Determinants of Health (SDOH) via integrated social services in the community.
Engagement with PharmD Live is designed to improve health outcomes with additional valuable benefits including:
- Patient education empowering disease self-management
- Telehealth convenience
- Reduction of out-of-pocket costs
- Fewer adverse drug events
- Fewer ER visits and hospital admissions
- Increased patient satisfaction and loyalty
Immediate benefits for providers
- Alleviates Medicare paperwork and practice workload
- Access to clinical pharmacists 24/7
- Added revenue stream
- Actionable clinical intelligence
- Increased patient loyalty
- Improved quality measures
- Empowering physicians and providing them with support
CMS quality measures impacted by our CCM
A turnkey metrics-driven Chronic Care Management solution that benefits your bottom line
- Positive quality payment adjustments
- Protects existing Medicare revenue
- Avoids Medicare penalties
- Exceptional performance status
- Negotiate favorable commercial payor contracts
CCM Implemenation Process
How PharmD Live’s CCM Process Works
Join growing practices using PharmD Live to improve patient outcomes
- No Upfront Cost
- We Assume the Workload
- Reduced Non-Billable Time
- Automated Patient Eligibility
