But They Don’t Have to Do It Alone
By Elliot Sternberg, MD
PharmD Live, Chief Medical Officer
The Center for Medicare and Medicaid Services (CMS) has embraced a framework created by the Institute for Health Improvement (IHI) designed to optimize the American healthcare system:
- Improve Patient Care
- Reduce Healthcare Costs
- Improve Population Health
CMS has aligned its Quality Payment Program metrics to increase (up to 7%), or reduce (down to 7%), physician reimbursements, tied to performance in pursuit of these goals. The Merit-Based Incentive Payment System (MIPS) has 4 performance categories (with weighting noted):
- Quality 45%
- Cost 15%
- Improvement Activities 15%
- Interoperability 25%
In addition, CMS has created a customized Advanced Payment Model (APM), featuring an overall financial risk component while requiring the use of a certified electronic health record (CEHRT) to receive a 5% incentive payment for groups of eligible clinicians focusing on specific clinical conditions, care episodes, or populations:
- Quality 50%
- Improvement Activities 20%
- Promoting Interoperability 30%
Though well intended, this initiative has placed a significant burden on primary care providers (PCP) who, for the most part, are paid on a productivity basis. The added administrative burden of detailed documentation, data collection and submission, in the setting of adoption of an electronic health record, has come at significant cost, time and stress for the health care provider and staff. It is not surprising that some older physicians have opted for early retirement, while others have joined larger organizations that can seemingly ease administrative burden. But the fact still remains – to be paid one must see patients and complete all of the necessary documentation, thus the pressure remains regardless of practice environment.
Consequently, physicians face a very “STEEEP” hill to climb in providing care to an increasingly aging and complex group of patients:

Is It Any Wonder Physicians Are Experiencing Burnout?
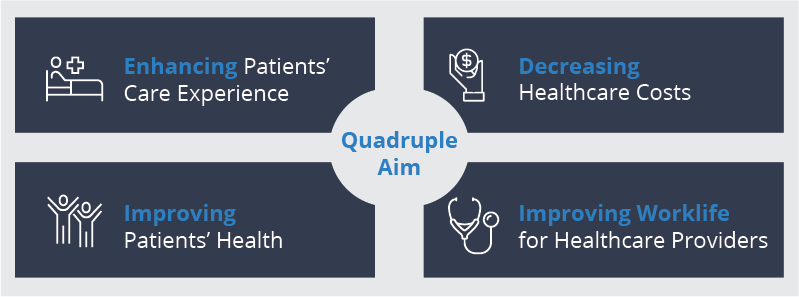
In response, healthcare providers should focus their efforts on realizing their own “Quadruple Aim”:
While The Solution To These Challenges May Be Complex, One Concept Rises To The Top:
The Primary Care Provider does not need to climb this very “STEEEP hill alone!”
The PCP should be finding greater personal and professional satisfaction when he/she practices to the maximum of their privileges and license. This strongly suggests the necessity of offloading many mundane tasks. This can be accomplished through collaboration with ancillary providers (pharmacists, behavioral medicine specialists, dietitians, and educators among others) which will enable the physician to focus on the diagnosis and management of more challenging clinical problems. Embracing a collaborative team approach, supported by effective technology and clinical apps, will help to overcome many of the STEEEP challenges they are forced to meet. Allowing others to assist will help improve and promote increased patient access, delivery of preventive services and education, and optimization of medication management while providing chronic disease management services between between physician visits.
The Result?
- Increased health of the patient and physician population;
- Enhanced experience of delivering and receiving care;
- Reduced per capita cost of care while rewarding primary care services.
For their own health and welfare, PCPs must explore different ways of meeting the needs of their patient population. Collaborating with others, embracing a team approach and adoptingsophisticated software solutions would be an effective start.








