Polypharmacy Definition and Risk Factors
Polypharmacy is most often defined as the simultaneous use of multiple drugs to treat a single medical condition. This often results in poor coordinated care for the patient because patients who live with multiple chronic conditions are more likely to have a decreased quality of life and self-rated health, lower mobility and functional ability. Furthermore, these patients have increases in hospitalizations, physiological distress, use of health care resources, cost, and mortality.
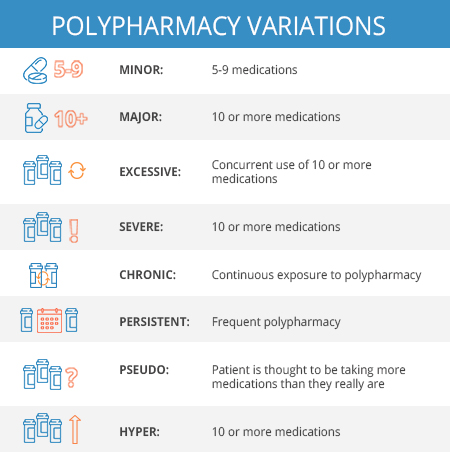
The term “polypharmacy” has also been associated with numerical definitions. Several studies have defined the number of medications fitting the criteria. Of these studies, 51 have defined polypharmacy as the use of ≥ 5 medications; while the second most common definition sited ≥ 6 medications. On the contrary, only one study for each ≥9, ≥10 and ≥11, have been said to fit the definition. Nonetheless, all studies sited a correlation between the increases in the number of medications taken with a rise in risk for adverse side effects.
Moreover, the rise in incidences where polypharmacy can occur may be attributed, in part, to clinical guidelines which often encourage the use of several medications to treat one medical condition. The impact of multiple medications being used for multiple conditions; however, is usually not studied in randomized controlled trials. In addition, predisposing determinants can also attribute to the rise in over medication. Such factors are defined as:
- Age (65 years and older)
- Sex (women)
- Education (lower levels of education)
- Hospitalizations (recent)
- Prescribers (more than one)
Given the number of studies on the subject, there remains a clear lack of one definitive definition of polypharmacy. This can prove challenging for healthcare professionals in evaluating the safety and efficacy of prescribing medications in a clinical setting.
The concern remains for Medicare patients undergoing chronic care management treatments as they commonly fall victim to polypharmacy. Professionals treating patients with chronic care needs should remain mindful of the increased risks of over medication by working with their patients to ensure a proper review of all medications prescribed. By being cognizant of the possibility for polypharmacy, healthcare professionals can help patients achieve better health outcomes.
References
- Masnoon N, Shakib S, Kalisch-Ellet L, Caughey GE. What is polypharmacy? A systematic review of definitions. Masnoon et al. BMC Geriatrics (2017) 17:230
- Sirois C, Laroche ML, Guenette L, Kroger E, Cooper D, Emond V. Polypharmacy in multimorbid older adults: protocol for a systematic review. Sirois et al. Systematic Reviews (2017) 6:104
- Rambhade S, Charkborty A, Shrivastava, Patil UK, Rambhade A. A Survey on Polypharmacy and Use of Inappropriate Medications. Toxicol Int. 2012 Jan-Apr; 19(1): 68–73. Retrieved June 23, 2019 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339249/
- Dwyer MO, Peklar J, McCallion P, McCarron M, Henman MC. Factors associated with polypharmacy and excessive polypharmacy in older people with intellectual disability differ from the general population: a cross-sectional observational nationwide study. BMJ Open 2016; pgs. 1-13.
Source:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339249/









One Response
Great article! Highly recommend!